LEFT FACIAL PARALYSIS
Name B jai Abhiram
Rollno 13
This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians sign informed consent.
CASE DISCUSSION
A 74 year old patient who is a resident of Narketpalli, a retired RTC driver has come to the OPD with chief complaints of
1) Body pains since 5 days
2) Vomitings since 2 days
3) Inability in swallowing of solids and liquids since 1 day
4) Slurring of speech since today morning.
HISTORY OF PRESENTING ILLNESS
30-8-2021
The patient was apparently asymptotic 5 days back. Then he developed
Generalised Body pains of duration 5 days, insidious in onset. He took medication from Local RMP and noticed no relief
Vomitings since 4 days of about 3 to 4 episodes everyday which are non bilious, non foul smelling, non blood stained, non projectile and contained undigested food particles.
Inability to swallow both solids and liquids since 1 day
Slurred speech since today morning which was sudden in onset and he is unable to move his Lower lip.
31-8-2021
The patient is doing fine. His body pains have reduced.
No Vomitings today
6-9-2021
The patient complains of pain of Right limb which is continuous probably a fasicular pain
He also developed right eye ulcers due to lagophthalmos
Discharged today
PAST HISTORY
1)He is a known case of Diametes mellitus-2 since 25 years.
He uses Mixtard twice daily
35 units in the morning
30 units at night
2) He is a known case of Cervical spondylitis since 10 years
3) He was a known case of Tuberculosis 3 years back.
He was given 3 bags of Blood. He started ATT and developed Diminished vision and recovered after a month. He stopped ATT due to loss of hunger after a period of 5 months and again restarted the course.
Total duration of ATT- 18 months
4) He had a fall 1 year back and has been using a stick while walking thereafter
He is not a known case of Hypertension, Asthma, Epilepsy, CAD and never had undergone through any surgeries
PERSONAL HISTORY
Diet - Mixed
Appetite - Normal
Bowel and bladder movements - Regular
Sleep - Inadequate due to body pains
Addictions - None
FAMILY HISTORY - Not significant
GENERAL EXAMINATION
The patient was conscious, coherent, Cooperative and well oriented to time place and person
He is moderately built and nourished
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing - absent
Edema - absent
Lymphadenopathy- absent
VITALS-
Temperature- 98.4 F
Pulse rate - 100/mm/min
Respiratory rate- 24 rpm
GRBS- 557
Spo2- 92%
SYSTEMIC EXAMINATION
CVS- S1 and S2 heard. No other murmurs heard
PA - Liver and spleen not palpable
Respiratory system- Normal vesicular breath sounds heard
CENTRAL NERVOUS SYSTEM EXAMINATION
Level of consciousness - Conscious
Speech - slurred
Memory - Immediate recent and remote memory present
Cranial nerve Examination:
1)Olfactory nerve - Perception of smell on both sides
2)Optic nerve - Counting finger positive from 6 metres
Visual field normal and colour vision is present
3)3,4,6 nerves- Pupils normal, ocular movements present, Nystagmus and Diplopoda absent
4)Trigeminal nerve- Prick and cotton wisp test positive
5)Facial nerve-
Deviation of mouth-
Frowning- present
Nasolabial fold- present
Blowing and Whistling- absent
Taste sensation- present
Corneal reflex- present
Clenching- present
NASOLABIAL FOLDS
FROWNING
CLENCHING OF TEETH
6) Vestibulo cochlear nerve-
Rinnes- positive
Weber- no lateralisation
7)Glossopharyngeal- gag reflex present
8) Spinal accessory- Shrugging of shoulders present
9) Hypoglossal nerve- no deviation of tongue
Motor examination
1)Inspection- Unable to completely extend his lower Limbs on supine position.
INCOMPLETE EXTENSION OF LOWER LIMBS
2)Palpation
a)Bulk- normal
b)Tone. Right. Left
Upper limb. Normal. Normal
Lower limb. Normal. Normal
c) Power. Right. Left
Biceps. 5/5. 5/5
Triceps. 4/5. 4/5
Extensor of leg. 4+/5. 4+/5
Flexors of leg. 4-/5. 4-/5
Extensors of hip. 5/5. 5/5
Doraiflexion of foot. 3/5. 3/5
Plantar flexion of foot. 3/5. 3/5
Extensors hallucinations longus- No movement on both sides
d)Reflexes
i )Superficial. Right. Left
Corneal +2. +2
Conjunctival +2 +2
Abdominal. +2 +2
ii )Deep. Right Left
Biceps. Hyperreflexive
Triceps Hyperreflexive
Supinator. Hyperreflexive
Knee. Hyperreflexive
Ankle Hyperreflexive
Sensory system
Superficial -fine touch, temperature, pain -present
Deep-position, vibration, crude touch, stereognosis, 2point discrimination- present
Cerebellum
Speech, nystagmus, ataxia, tremors, released reflexes absent
Coordination and gait
Finger nose test , finger finger test, heel knee test-present
Gait -dragging type
Romberg test -negative
Signs of meningeal irritation
Nuchal rigidity,kernigs and brudzinski’s sign - absent
Neck rigidity is present due to ossified posterior longitudinal ligament - cervical spondylitis.
CERVICAL SPONDYLITIS
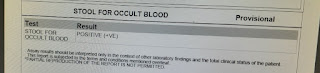
INVESTIGATIONS
X RAY NECK
CT BRAIN
ECG
USG ABDOMEN
2D ECHO
OPHTHALMOLOGY CROSS CONSULTATION REPORT

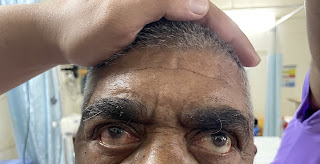
Picture taken on 30-8-2021
Picture taken on 6-8-2021
PROVISIONAL DAIGNOSIS:
Left sided facial paralysis
TREATMENT:
Day 0:
1. Inj.HAI 39ml +1ml HAI @6ml/hr til grbs is <200mg/dl
2. Tab.Ecospirin
3.tab.clopidogrel
4. Atorvastatin/49mg/Po/Od
5. GRBS 1hrly
Day1
1.Tab.Ecospirin
2.tab.clopidogrel
3. Atorvastatin/49mg/Po/Od
4. Inj. HAI/SC/TID (8am--X--8pm)inform sugars to icu pg
5. Inj NPH/SC/BD
6.TAB.ULTRACET 1/2 TAB PO QID
7.INJ.TRAMADOL 1Amp in 100ml NS IV SOS
8. IVF- NS @75ml/hr
9.GRBS















Comments
Post a Comment