80 year old male patient came to OPD with cheif complaints of generalized body pains since 2 months
This is an a online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitt.
Cheif complaints
1)Complaints of Generalized body pains since 2 months.
HOPI:
Patient was apparently asymptomatic until the age of 15 years then history of:
1)Hemoptysis
2)cough(productive)
3)Fever
4) Weight loss and diagnosed to have Tuberculosis and took treatment for 6months(till sputum -ve)
Age of 20 years:Similar complaints and patient had recurrence of pulmonary Tb and started on ATT for 9 months and confirmed with sputum -ve.
At age of 40 years: Patient devloped lesions on the skin which initially started as small swellings(painful) and then progressed to the present size(painless) and multiple on both upper and lower limbs.
At age of 50 years: Patient developed constipation not associated with pain abdomen, vomiting and Malena.
1-2 years ago patient developed polyuria,polydypsia,polyphagia and pain at limbs and diagnosed to have HTN and started with Telma.
HO Past illness:
2 months ago patient had similar complaints and pain at all limbs,dragging type of pain, sometimes associated with tingling and numbness ,pain is increased with activity and reduced with rest, associated with weakness of limbs and no restriction of movements,no loss of power.
N/k/o of epilepsy, Asthama,DM.
Personal History
Diet:Mixed
Appetite:Normal
Bowel and bladder movement: Normal
Sleep: adequate
Addictions:smoked chutta for 40 years and stopped it for past 12 years.
Nutritional History:
Morning: Breakfast- idli (sambar and chutney)
Afternoon -Rice with sambar and curd.
No snacks
Dinner-curd rice with curry and pickle.
On examination:
Patient is C/C/C with time place and person.
No pallor ,icterus cyanosis and generalized lymphadenopathy.
Clubbing:+
Slip sign+
Transilluminated
Skin-smooth
Vitals
BP:110/80
PR:92bpm
RR:18cpm
Temperature:98.6f
Cvs:S1 and S2 heard
R/S:BAE+
Pectus excavatum+
CNS:NFND
P/A:
Inspection
Shape of abdomen:Distended
Umbilicus-central and inverted
No visible scars ,sinuses,dilated veins.
Hernial orfices normal.
Palpation
No local rise of temperature
No gaurding, rigidity,rebound tenderness.
No hepatomegaly and splenomegaly
Percussion:Resonant
Liver span -Normal
Auscultation:
Bowel sounds -+
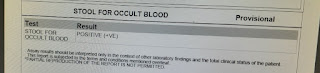
Investigations:
CBP
Hb-13.4
Tlc-8600
Rbc-4.47
Plt:2.32lakhs
Blood urea-22mg/dl
Serum Na:135
Colour Doppler
ECG
Treatment
1)Tab ultracet 1/2 Qid
2)Tab MVT OD
3)Tab Telma 40mgOD








Comments
Post a Comment